Did you hear the good news about Native American elders? They are living longer, healthier lives than ever before. Yes, life expectancy is still lower than other U.S. racial/ethnic groups. But that’s improving. While there were only 42,000 Native elders over age 85 in 2012, Tribal nations are expected to have 300,000 by 2050.
But there’s one area that hasn’t caught up with this increase: resources. Just like any other seniors, Native elders often need consistent care – but Native communities often have limited healthcare options. There just aren’t many skilled nursing facilities on Tribal lands. Hospice care? Even rarer.
Long-term care staff also need to remember that Native elders experience the same health disparities as any Indigenous person. Diabetes, cardiovascular disease, hypertension, and kidney disease are all higher in Tribal nations. Alcoholism-linked dementia is on the rise among Indigenous elders too.
But there’s an even bigger factor impacting the Native experience in long-term care facilities – culturally responsive care.
The Dynamics of Difference: Caring for Native Elders
While old age may not be easy for anyone, Native elders often carry a lifetime of systemic racism and cultural erasure. They may have lost their language, culture, health, family, land, or ancestral teachings. A history of generational trauma and poverty can impact their health – particularly as many elders are survivors of abusive boarding schools.
These experiences affect Native elders today. Consider a CNA who asks a resident why she didn’t eat her vegetables. The resident, a boarding school survivor, associates the question with “wasting food” and “being in trouble” and becomes agitated. Or a provider who teases his male patient about his extremely long hair – not understanding the patient’s tribal members only cut their hair after the death of a loved one.
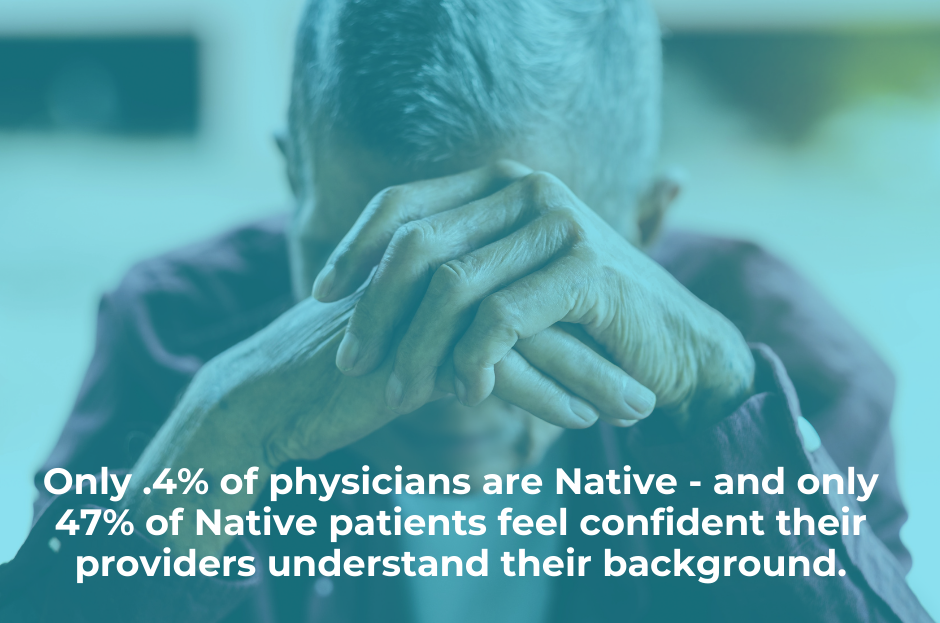
This kind of encounter can alienate Native patients – which is hardly surprising, considering the long and troubled history between Native communities and the medical industry. From forced sterilization to medical experiments to healthcare fraud, many Native patients have good reasons to distrust providers. But where your average patient can go home after a doctor’s visit, Native elders in long-term care are enveloped in a 24/7 healthcare experience with mostly non-Native providers.

5 Practices for Culturally Responsive Long-Term Care
So how do we bridge the dynamics of difference? Every resident or patient a skilled nursing or long-term care facility will have unique needs, of course – but these 7 practices can help keep Native seniors culturally connected and comfortable in their golden years.
Accept feedback.
This can be a tough one. But even healthcare workers with the best intentions can misstep when caring for someone of a very different background. When this happens, it’s natural to receive some advice – or even a gentle correction – from coworkers and residents. If this happens to you, don’t take offense; just show your willingness to learn and provide great care.
Be patient.
Sometimes you’ll encounter a patient or resident who seems to be testing you. Chances are, they’ve probably been treated poorly before in a clinical environment and now they are assessing whether you can be trusted. Other times a family member will express frustration. Usually this is an expression of their own guilt at “putting their loved one in a home” rather than a response to anything you’ve done.
Communicate respectfully – and don’t rush.
Native people often report that providers rush them through encounters or cut them off mid-sentence. And no doubt you’ve heard of the “doorknob moment” where patients blurt out their questions right as you’re exiting the exam room. Give your patients and residents time to think about their answers and ideas; listen to what they say and give them time to ask questions.

Study trauma-centered care.
Native patients or residents may react to their loss of freedom and control in a long-term facility. Whether they’re being told to eat a specific food or being helped to a bathroom, they may be reminded of past traumas and respond accordingly – especially if they’ve survived boarding schools or grown up in families impacted by them. Some of their behavior might include:
- Feelings of disconnection and not belonging
- Anxiety and depression
- Disordered eating issues
- Bathroom assistance problems and other sexual abuse responses
- Suicidal ideation
Our best advice: study trauma-informed care. One way you can help your residents is to find ways they can use their voice and exercise their autonomy to help them feel more in control of their healthcare experience.
Prepare for end-of-life care.
End-of-life transitions with Native residents and patients can look a little different. Before proceeding with a “standard” death process, ask the resident’s family about their preferences. You may have a large gathering and a steady stream of visitors who want to pay their respects. Some families may reject embalming or want the resident to wear special clothing or be buried with ceremonial objects. Hearing is often one of the final senses that remain near death; feel free to ask families if they have tribal songs or recordings to play at their loved one’s deathbed.
Everyone deserves comfort and respect as they grow old. Creating more long-term care facilities on Tribal nations is a worthy goal but one that can’t be achieved overnight. What can be changed now is our approach to Native American elder care – and ensuring Native seniors enjoy the same chance for dignity and peace as any other senior.

