by Ryan Scott
It’s World Diabetes Day – and diabetes is a major public health crisis that disproportionately affects Native American communities, with rates three times higher than the general U.S. population. This has a devastating impact on the health and well-being of these communities.
Understanding Diabetes
Diabetes is a chronic disease that affects how the body turns food into energy. When a person has diabetes, their body either resists the effects of insulin or doesn’t produce enough insulin. Insulin is a hormone that helps the body’s cells use glucose for energy. There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease that occurs when the body’s immune system attacks and destroys the cells in the pancreas that produce insulin. Type 2 diabetes is the most common form of diabetes and is caused by a combination of genetic and lifestyle factors.
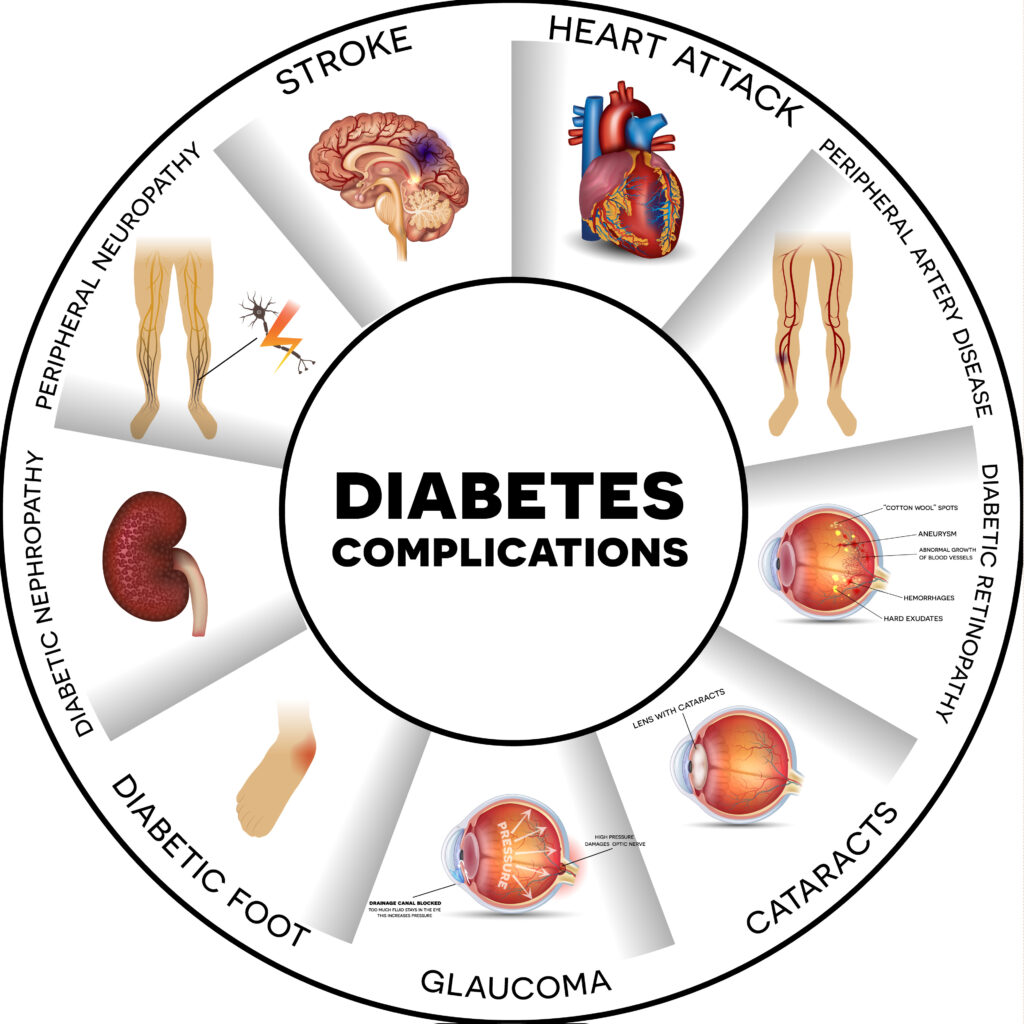
Native people with diabetes are more likely to develop serious health complications earlier in life and at a higher rate than the general U.S. population. These complications include heart disease, stroke, blindness, kidney failure, and amputation. Diabetes is also the leading cause of death among Native American people. They are two to three times more likely to die from heart disease and stroke than the general U.S. population and three times more likely to develop end-stage renal disease (ESRD), which is a condition that requires dialysis or a kidney transplant.
Diabetes in Indigenous America
The extent and severity of diabetes on Tribal lands is staggering. According to the Indian Health Service (IHS), over 25% of Native adults have diabetes, which is more than twice the rate of the general U.S. population. Diabetes can be a major contributor to poverty, unemployment, and disability in Native communities. It can also disrupt traditional lifestyles and cultural practices, leading to social isolation and depression.
There are a number of factors that contribute to the high rates of diabetes among Native people, including genetics, lifestyle factors, and socioeconomic factors. Native people are more likely to be obese, a major risk factor for type 2 diabetes. They are also more likely to have unhealthy diets and be physically inactive. Native people are more likely to live in poverty and have less access to healthy food and opportunities for physical activity. They are also more likely to experience discrimination and racism, which can lead to stress and poor health outcomes.

Preventing Diabetes
Diabetes prevention programs can take a number of approaches, such as improving access to healthy food and opportunities for physical activity and addressing the root causes of the disease. Some programs that are working to address this crisis include the Special Diabetes Program for Indians (SDPI) and the Diabetes Prevention Program (DPP) implemented by the Indian Health Service (IHS) and the Diabetes Prevention and Control Program (DPCP), implemented by the Centers for Disease Control and Prevention (CDC). In addition to these government programs, there are a number of community-based organizations that are working to address diabetes in Native communities.
Does your facility offer diabetes prevention programs? A good first step is educating patients about diabetes and the factors that contribute to it; another is collaborating with community organizations that support diabetes prevention and care for Native people. Together, we can make a positive impact on the health and well-being of Native communities and the care received.


